Strategies to Combat Cognitive Fatigue
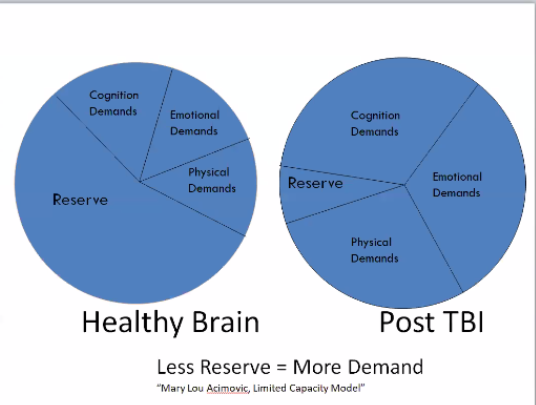
Co-founder of The Brain Injury Hope Foundation Mary Ann Keatley explains the Energy Pie during the October 2020 Survivor Series via Zoom.
By Eliza Marie Somers
We’ve all experienced exhaustion: When we are so tried after a long day we just […]