Dr. Danny Mistry uses a team of healthcare professionals to help brain injury survivors.
By Eliza Marie Somers
As a brain injury survivor, do you sometimes feel as if you’re spinning your wheels dashing to vision therapy to vestibular therapy to speech therapy? It’s no wonder mTBI survivors experience fatigue, especially when you add in daily chores such a cooking, cleaning and grocery shopping.
Dr. Danny Mistry just may hold the key to the future model of brain injury therapy at his clinic in Fort Collins, Colorado
During the Brain Injury Hope Foundation’s Aug. 11, 2023, Survivor Series: “Dr. Danny Mistry’s Aasha Brain Clinic: Neurodiversity, Concussion, and Brain Injury,” Mistry revealed his strategy to help TBI survivors.
- Danny Mistry
Aasha Brain Clinic
2021 Battlecreek Drive, Unit A
Fort Collins, CO 80528
833-992-2742
[email protected]
https://aashabrainclinics.com/ - Mistry will be glad to speak with anyone who calls and needs help to guide them, knowing that he cannot offer direct medical help without establishing a doctor – patient relationship. Within the confines of his part-time schedule, he is glad to evaluate them as a patient and that he accepts only Medicaid, Medicare Part B (only).
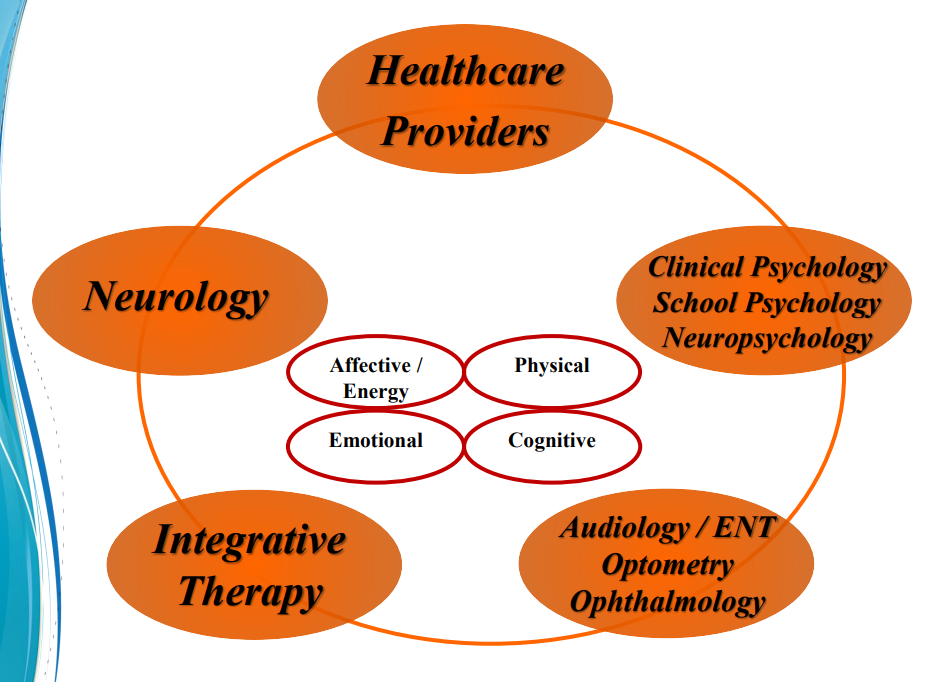
“It takes a team approach to provide comprehensive concussion management” explained Mistry, who is a National Team Physician and Chair of the Concussion Task Force for USA Swimming.
Mistry’s brain clinic features several independent health care providers under one roof, where patients will find a wealth of information, services and therapies. The Aasha (which means “Hope”) Clinic features:
- Mistry, an internist with specialties in sports medicine and exercise science.
- Karen McAvoy, who is dually credentialed as a clinical psychologist and school psychologist.
- Nicole Crawford, a licensed psychologist and school psychologist.
- Colorado in Motion, offers occupational therapy, vestibular therapy, and speech language therapy/cognitive therapy.
The team approach Mistry implements also involves parents, teachers and coaches if the survivor is involved in sports. “We need to address the brain in its entirety,” he explained. “It’s about access to care. The evolution of medical management has changed over time.”
“It’s been a gift of a lifetime like no other to take care of brain injury survivors. It’s humbling to take care of people with concussions.” – Dr. Danny Mistry
Before Mistry moved to Colorado, he was the team physician and co-medical director for the University of Virginia athletic department. While at Virginia, Mistry developed numerous sports medicine programs for Division I athletes, including concussion protocols.
“With a team approach, we provide hope,” Mistry said. “I’ve learned that the brain is the most complex and paradoxically, the simplest organ. In health, when firing on all cylinders, it’s amazing what a brain can do. And we also know how devastating it is to individuals who are injured.”
Mistry and his team use a CARE model when treating brain injury patients.
CARE stands for:
- C: Communication, Commitment to excellence, Consistency of care.
- A: Affordability, Awareness, Access to care.
- R: Resolve, Respect for individuality.
- E: Education, Expeditious care, Evolution – address the importance of adaption to change of the principles of medical management over time.
“The fact that help individuals heal from brain injury is commitment to excellence every day,” Mistry said. “I think that’s the key piece, and that it starts with good communication. I am lucky doctor who practices in this clinic, across the hallway from accomplished clinical and school psychologists, occupational, vestibular and speech language therapists. … And I think aspiring to having more models of this across the country is going to help brain injury globally.”
Hope is Key to Aasha Clinic
Mistry confirmed what many mTBI survivors know, and that is there is nothing mild about the impact of a mild traumatic brain injury, aka concussion. The term MILD is misleading and frustrating to many mTBI survivors as symptoms can last for years, and some people may experience symptoms weeks after the initial injury.
However, Mistry stressed there is hope for the brain injury survivor and their families because of the brain’s ability to rewire neuro pathways, aka neuroplasticity, a term that was foreign to doctors not too long ago. “There’s always hope and there’s something we can always do for folks,” he said.
Call to Action
- Danny Mistry urges brain injury survivors to
- Stay active physically and cognitively
- Eat antioxidant foods
- For more antioxidant foods
Along with neuroplasticity, Mistry also embraces neurodiversity, which is the differences in individuals’ brains and behavioral traits or to put it simply – the unique ways in which people’s brains work.
“Neurodiversity is based on the fact all our brains are different,” Mistry explained. “How boring would it be if everyone’s brain was the same. There would be no fun in life. There is a range of differences in individual brain function and behavioral traits. … We (the medical community as a whole) typically do not embrace this concept when treating folks with mTBI.
“Each individual presents differently. They (injuries) might be similar, but clinical presentations are not the same. … And expecting a standard pattern of clinical presentation of recovery is unrealistic.”
Mistry stressed that a failure to embrace the concept of neurodiversity in treating individuals with brain injuries is against the clinic’s principles of good patient care, and that expecting a standard pattern of recovery in ALL individuals is unreasonable and unrealistic.
“It’s incredible how different brain injuries affect people differently,” he said.
Mistry explained a brain injury is a complex “processing dysfunction” that can affect a survivor’s physical well-being, emotional well-being, and the ability to think clearly. Some common symptoms of this dysfunction include:
- Mental fatigue
- Sleep disturbances
- Headache
- Balance problems
- Eye, ear and stomach symptoms
- Depression
- Anxiety
- Changes in behavior and personality
- Difficulty concentrating
- Memory problems
- Slow processing
- Mental fogginess
And all these symptoms can overlap, requiring numerous therapies in order to correct the “processing dysfunction.” “The brain is sitting in fluid surrounded by cerebral spinal fluid,” Mistry explained. “The brain is not attached to the skull, it is floating, so it doesn’t take much for this Jell-O like organ containing a hundred billion nerves cells to get damaged.”
Dr. Danny Mistry says rehabilitating the root of the brain injury is key to successful recovery.
Lack of Communication in the Brain
Even though each brain injury is different, “the net effect is the same – it’s a lack of communication between neurons,” Mistry said. “It’s a change in the energy function of the brain depending on which lobe it affects.
“If the brain isn’t communicating then good things don’t happen. People develop symptoms because of a miscommunication in the brain. … There are physical and chemical changes in the brain.”
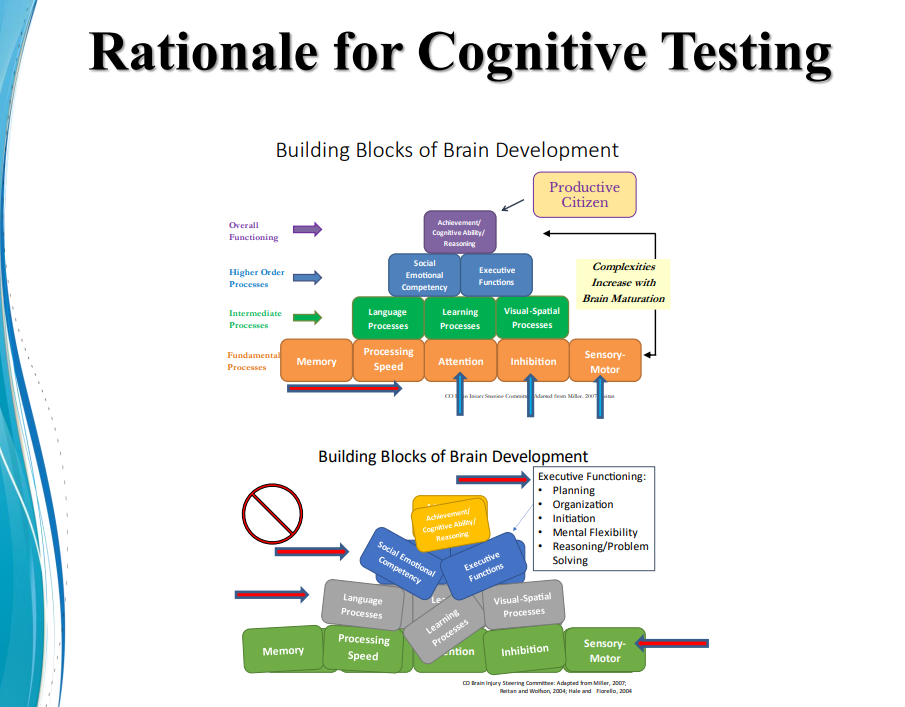
Mistry referred to a diagram featuring the building blocks of the brain to illustrate what happens when one part of the brain is impacted by an injury
“When you think of the building blocks of the brain, the fundamental processes are memory, processing speed, attention, inhibition, sensory order. These complexities increase as we grow from childhood to adulthood. And then the intermediate processes are dependent on these fundamental processes, which include language, learning and vision spatial.”
Finding the Root of the Problem
“If you think about a healthy tree as a concept of health and recovery from mTBI concussion, it begins with knowing what’s in the roots. It begins with the root and ends with the leaf, so to speak. And everything in the trunk to me is the rehabilitation. Water the roots correctly and get to the bottom of the problem in the roots, and then you can have a healthy tree.”
– Dr. Danny Mistry
As a person matures, they develop good social skills, emotional competence and executive functions, which include planning, organization, initiation, flexibility, reasoning and problem solving. However, when a concussion occurs all of these processes are impacted negatively because the root functions are negatively impacted.
“It’s a myth to think we can separate common brain dysfunctions, but in reality, the symptoms overlap. … It’s all interconnected,” Mistry said. “And these symptoms create impairments in cognitive function, vestibular function. … and leads to psychological problems, sleep problems, anxiety, depression.”
Mistry urges early neurocognitive testing to determine what type of care will benefit a survivor, along with post-injury testing to evaluate progress and for possible changes in therapies. He also urges testing BEFORE a brain injury when a person is healthy to help assess changes in case of a future injury.
“There’s nothing simple about brain rehabilytation,” he said. “We all know that. But what is true is a comprehensive evaluation is critical, just like anything else in medicine. It’s an essential piece.”
A majority of brain injury survivors experience vision and vestibular issues after an injury.
The Eyes and Ears Work in Unison
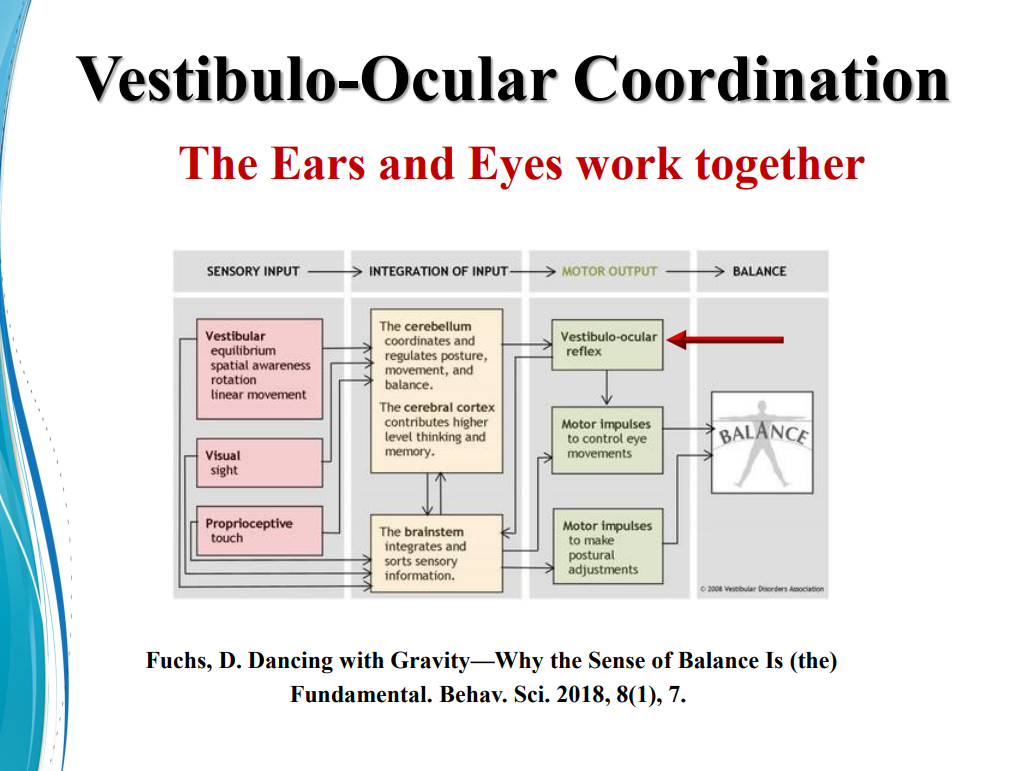
Vision therapy and vestibular therapy go hand-in-hand, Mistry explained, as the ears and eyes are complex systems that work together for many functions, including balance, memory, motor control and sensory processing.
He stated that 85 percent to 90 percent of brain injury survivors have some element of ear and eye dysfunction, and early assessment is a big key to regaining a healthy brain.
“The ears work with the eyes, and if they are not working together, then the brain in not working right,” Mistry said. “Contrary to common thinking that the inner ear is more related to balance, actually, the inner ear is also very important for cognition because it works with the eyes to provide the brain with good input.
“So, you have to think about the root of the cognitive dysfunction in the eyes and ears because there’s delayed visual memory, which leads to delayed processing.”
Mistry said he’s seen a “tremendous difference” in survivors who address vision and vestibular issues.
Vestibular (or ear) dysfunction can present with the following symptoms and signs:
- Feeling of slowed down.
- Difficulty concentrating.
- Light and sound sensitivity.
- Memory problems.
- Balance problems.
Post-trauma vision syndrome can present with the following symptoms and signs:
- Eye misalignment.
- Convergence issues.
- Trouble focusing.
- Spatial distortions.
- Delayed memory/processing.
- Midline shift.
- Involuntary eye movement.
- Blurred or double vision.
- Gait issues.
- Inability to concentration.
- Difficulty reading and comprehension.
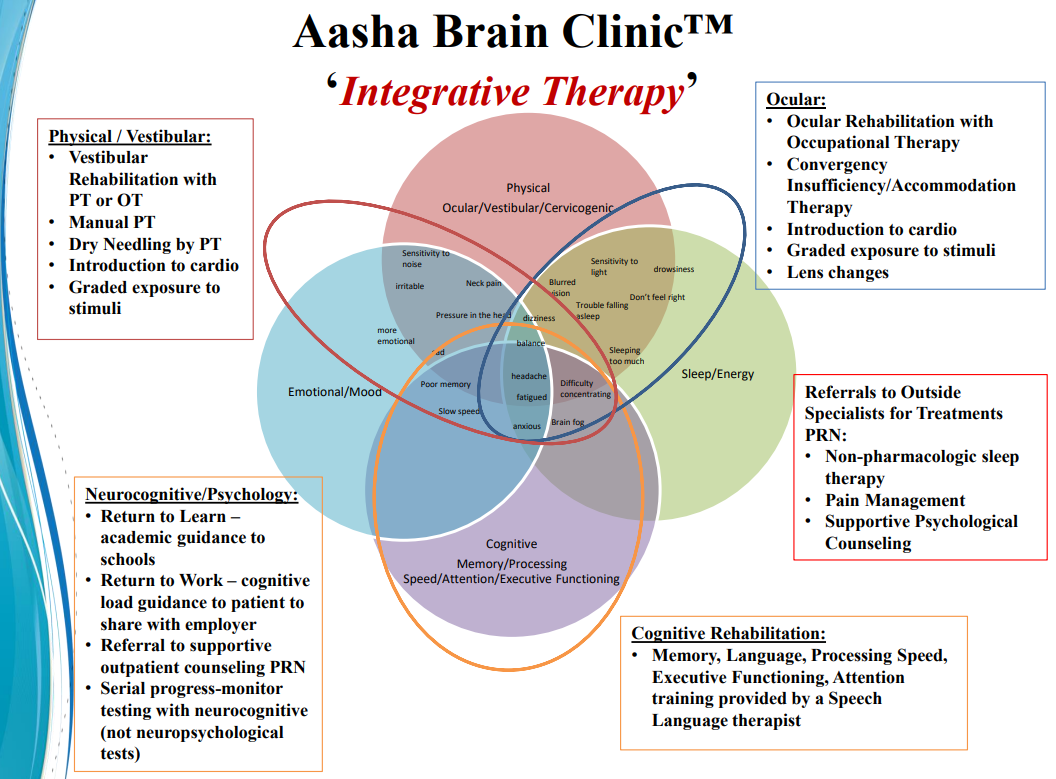
Mistry uses an integrative evaluative and therapeutic approach to care for his patients with brain injury.
Integrative therapy is a key component of the Aasha Clinic.
Calling the Signals
Mistry described his role at the Aasha Clinic as a quarterback calling the plays.
“I think of myself as the quarterback in trying to orchestrate care, helping to coordinate referrals, looking at information from imaging studies, cognitive testing, etc., and trying to apply that to the patient’s symptoms into objective measures of function.”
“It’s not complex. These are the basis of good recovery. And easier said than done,” he said.
“We need to aspire to create clinics where we have integrated rehabilitation under one roof. We strive for that at the Aasha Clinic. And in the perfect world of concussion management, I wish we had centers everywhere under one roof.”
“Better is possible. It does not take genius. It takes diligence. It takes moral clarity. It takes ingenuity. And above all, it takes a willingness to try.”
— Atul Gawande,
Surgeon, Writer, Health Adviser
link https://atulgawande.com/